Nga Maia Maori Midwives Aotearoa was formed in 1993 by Māori midwives, midwifery tutors and their students, to address the inconsistencies in maternity services for Māori in New Zealand. Registered as a charitable trust in 1994, Nga Maia became recognised in maternity circles as the ‘voice’ for Māori. By 2008 its role was endorsed by the Midwifery Council of New Zealand (MCNZ), the New Zealand College of Midwives (NZCOM) and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG). [1] Nga Maia’s mission was to: support the retention and recruitment of the Māori midwifery workforce; promote and protect the tikanga values of traditional Māori birthing and parenting knowledge; and support Māori whānau to achieve an equitable, clinically and culturally safe birthing and mothering experience. [2]
Rather than increasing, the Māori midwifery workforce declined slowly throughout the 1990s and 2000s. Successive governments were apparently unwilling or unable to address this problem. Nga Maia was determined to support the dwindling numbers of Māori midwives scattered sparsely throughout the country.
The organisation was dedicated to improving the recruitment and retention of Māori midwifery students, by ensuring that their learning and cultural needs were being met. It consistently attempted to make changes that would build the Māori maternity workforce, increase support for Māori midwifery students, and recall and reassert the traditional birth practices of their forebears, so as to assist and enlighten pregnant Māori women in order to deliver better outcomes for them and their babies.
Nga Maia Maori Midwives Aotearoa
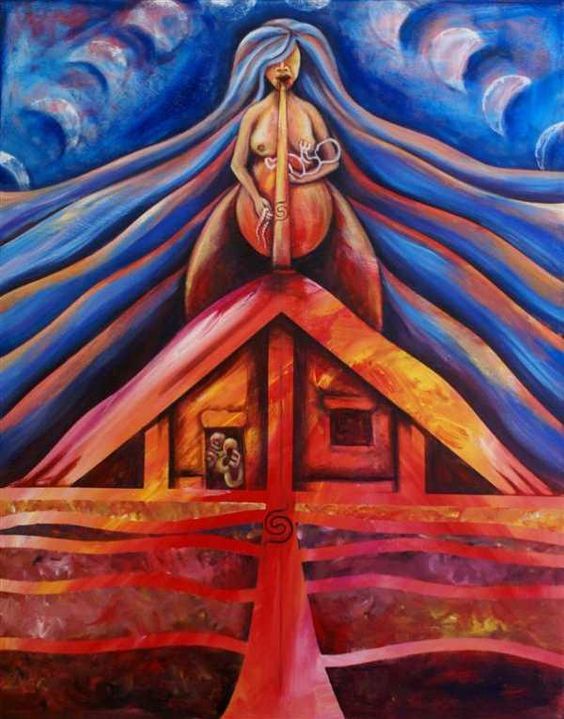
Strength from my Ancestors – Hine Te Iwaiwa, created by Regan Balzer for Nga Maia o Aotearoa.
The Nga Maia Trust was governed by five elected board members, two from the South Island and three from the North Island, serving for a term of three years. From 2014, it was managed by a volunteer CEO, administering the day to day needs of its members and reporting directly to the board each month. Apart from a part-time administrator’s salary, there was no other financial compensation for the efforts of those involved.
Five well-established rōpū adopted the Nga Maia Charter: Northland–Auckland, Hamilton, Hawkes Bay–Wairoa and Gisborne, Wellington, and Christchurch. Each rōpū was aligned with a specific District Health Board (DHB) area, and each determined their own regional membership, based on whakapapa. The Planned Strategic Goal of each rōpū was to ensure that a Nga Maia representative was actively involved on each DHB to ensure a Māori voice was heard in supplying maternity, parenting and midwifery services, recognising traditional Māori birthing tikanga, supporting Māori midwifery workforce development and supporting access for Māori whanau.
Each rōpū was also actively engaged, through a tuakana/teina mentoring model, in providing support for Māori midwifery students and Māori new graduate midwives in their first year of practice. Through its head office, Nga Maia also managed the various committee advisory roles demanded of its members.
Rōpū member lists were updated and sent annually to head office, which then maintained a membership database. In 2019, Nga Maia had 275 financial members. They included Māori midwives and midwifery students, whanau and kaumatua, who self-determined their whakapapa links to hapū and iwi throughout Aotearoa.
However, funding was a difficult issue. Voluntary membership fees, set by each rōpū individually, were retained by the rōpū to finance their own administration needs. Nga Maia’s income as an organisation, assessed annually, was thus dependent on variable funding from the Ministry of Health’s Māori Provider Development Scheme.
Financial stability for Nga Maia was therefore not guaranteed. The inflexibility of the funding process, and the unpredictable size of the annual grant, together with the need to rely on volunteer staff, meant that Nga Maia could not count on having the resources necessary to pursue its core goals. Requests that NZCOM pass on to Nga Maia a share of the annual membership fees ($695 per year in 2018) paid by those Māori midwives who self-identified as Nga Maia members had not met with success.
Yet research repeatedly highlighted the continuing disparities in maternity care and outcomes for Māori, and emphasised the value of cultural competency. A 2013 report, Hapu ora: wellbeing in the early stages of life, stated that:
Māori mothers and their babies experience considerable disparities compared to New Zealand European mothers and babies, including persistent differentials in low birthweight, preterm birth, SGA [small for gestational age], stillbirth and neonatal deaths. Having a higher prevalence of maternal risk factors compared to other women means Māori women have greater maternity care needs. [3]
This review identified ‘gaps in knowledge about best practice in maternal and newborn service delivery, particularly in relation to the contribution of Māori knowledge to the planning and development of mainstream initiatives’. It concluded that:
Both quality of care and whānau experiences of care affect birth outcomes and health seeking behaviours, throughout pregnancy and beyond . . . Some services appear to work well for Māori whānau while others do not. The variability in care experiences found in the literature was reinforced during the sector engagement process, with Māori knowledge, practices and practitioners seen as having considerable potential to inform service delivery. [4]
In 2007 Nga Maia established Turanga Kaupapa, a ‘cultural framework’ for maternity.
The Turanga Kaupapa Cultural Training Workshops were endorsed by NZCOM as a compulsory midwifery competency, supported through the Midwifery Standard Review (MSR) process. A review in 2017 resulted in the development of a workbook, and Turanga Kaupapa workshops being held for every midwifery school and all midwives working currently in New Zealand. The workshops were run by trained and endorsed Nga Maia facilitators. Registered Nga Maia members attended free; non-members, including DHB midwifery staff, paid $150 each. The income received was used to fund flights, accommodation and meals for the facilitator.
The numbers of Māori babies taken into state care within three months of birth caused concern among Maori midwives and whanau. These numbers had increased from 129 in the year to June 2016 to 160 in each of the two years to June 2018 – over three a week. The numbers of babies of all other ethnicities taken into state care had increased only slightly in the same period, from 118 to 121. [5] After an incident involving the attempted uplift of a 6-day-old baby from his 19-year-old mother in a Hawke’s Bay hospital received media publicity, [6] three enquiries were set up. [7]
By 2019, a total of 320 Māori midwives (just under 9 percent of all midwives) held an annual practising certificate (APC) and were registered with the Midwifery Council. Of these, 165 were working as Lead Maternity Carers, and another 100 were working in DHBs. About 40 were working overseas, mostly in Australia. [8]
Māori midwives reported continuing to find that their applications for employment were often unsuccessful, with apparently no recognition of their cultural value within the service. In 2019, none of the five midwifery schools had any Māori midwifery tutors, and only one of the 21 DHBs had a Māori midwifery advisor. The Ministry of Health had a Māori Director of nursing, but no Māori Director of Midwifery. [9]
This inequity was seen as related to dysfunctionality in decision making for Māori needs, and no consistency in planning outcomes for Māori within maternity services. With no guarantee of participation, representation or commitment at a strategic level, Nga Maia believed it would continue to struggle to achieve equitable outcomes in maternity and child health services for Māori, despite being nominated to do so and supported by its members, Māori midwives and Māori whanau throughout New Zealand. [10]
Jean Te Huia [11]
Notes
[1] Te Huia, Jean, 2018.
[2] Te Huia, Jean, 2018, 2019. Information about Nga Maia is derived from these sources unless otherwise stated.
[3] Moewaka Barnes, Helen, et al., 2013, pp. 74–5.
[4] Ibid.
[5] See Neilson, Michael, ‘Oranga Tamariki social worker apologises after “joke” to mum about bonuses for uplifting children’, NZH, 17 June 2019, https://www.nzherald.co.nz/hawkes-bay-today/news/article.cfm?c_id=1503462&objectid=12241144&fbclid=IwAR1Mdb3oclsF3zxcy19Ugu9zyrslbk998H3t31QV0LNDOTlJgfN91bWXnsc
[6] See, for example, Reid, Melanie, ‘Taken by the state: Don't take my baby’, Stuff, 9 May 2019, https://www.stuff.co.nz/national/112568714/taken-by-the-state-dont-take-my-baby?rm=m
[7] See ‘Ombudsman unveils inquiry into Oranga Tamariki newborn uplifts’, NZH, 19 June 2019; Hon. Tracey Martin, ‘Oranga Tamariki Review’, press release, 18 June 2019, https://www.beehive.govt.nz/release/oranga-tamariki-review
[8] Te Huia, 2019.
[9] Te Huia, 2018.
[10] Ibid.
[11] Nga Maia CEO in 2019.
Unpublished sources
Te Huia, Jean, ‘Disparities for Māori within the Maternity System’, paper presented to New Zealand College of Midwives Conference, Rotorua, 2018
Te Huia, Jean, informal notes, May/June 2019
Published sources
Moewaka Barnes, H., et al., Hapu ora: wellbeing in the early stages of life, Massey University for Health Research Council and Ministry of Health, 8 Nov. 2013, http://www.massey.ac.nz/massey/fms/Colleges/College%20of%20Humanities%20and%20Social%20Sciences/Shore/reports/Hapu%20Ora%208%20Nov%202013.pdf
Rhind-Wiri, Hinerangi, ‘Where is the support for Māori midwives?’, The Spinoff, 8 May 2018
Further sources
Nga Maia Māori Midwives Aotearoa website: https://www.ngamaia.co.nz/


Community contributions